(MainsGS2:Government policies and interventions for development in various sectors and issues arising out of their design and implementation.)
Context:
- There is a strong tendency in public health to prioritize individual-oriented interventions over societal oriented population-based approaches.
Individualism in public health.
- Data from the National Sample Survey Organisation (75th round) show that on an average, only 3% of the total population in India had an episode of hospitalisation in a year.
- Ideally, the Government needs to ensure health-care facilities to only 3%-5% of the population to cover all the hospitalisation needs of a population.
- However, instead of giving an assurance to every individual without ensuring the necessary health-care services to the population is not really helping in a crisis.
- This was evident in an evaluation of publicly-funded insurance schemes, which points to the low proportion of population that benefited from the scheme annually.
Approach of PMJAY:
- A nationwide publicly-funded insurance scheme, the Pradhan Mantri Jan Arogya Yojana (PMJAY) falls under Ayushman Bharat.
- It is the largest health insurance scheme in the country covering hospitalisation expenses for a family for ₹5 lakh a year.
- The goal is to ensure ‘free’ curative care services for all kinds of hospitalisation services so that there is no financial burden to the beneficiary.
- Instead, every individual is given an assurance that if there is a need for hospitalisation expenses, the scheme will cover the expenses, highlighting the risk/probability of every individual facing hospitalisation in a year.
- This is an individualistic response to the problem of hospitalisation expenditure faced by populations as this becomes obvious when one examines the data on annual hospitalisation across populations.
Dominance of individualism:
- The dominance of biomedical knowledge and philosophy in the field of public health with a misconception that what is done at an individual level, when done at a population level, becomes public health.
- This is despite the contrasting philosophy and approaches of clinical medicine and public health and the evidence that support the latter and must be based on population characteristics and economic resources.
- Health effects are more visible and appear convincing at the individual level, wherein improvements at the population level will be clear only after population-level analysis; this needs a certain level of expertise and orientation about society — an important skill required for public health practitioners.
Risk and susceptibility:
- The beneficiaries for a programme become the maximum when 100% of the population is targeted.
- On the contrary, from a population perspective, the actual beneficiary will reduce to only 5%-10% in case of hospitalisation services and 20% of those affected with COVID-19 for treatment needs.
- Instead of making efforts to supply evidence of the actual prevalence of public health problems, market forces would prefer to cast a wide net and cover 100% of beneficiaries.
- Propagating individualism has always been a characteristic feature of a consumerist society as every individual can then be a potential ‘customer’ in the face of risk and susceptibility.
Conclusion:
- All forms of individualistic approaches in public health need to be resisted to safeguard its original principles of practice, viz. population, prevention, and social justice.

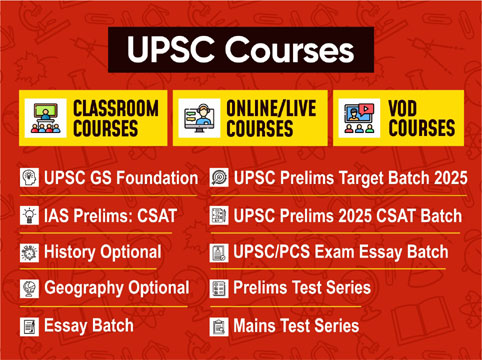
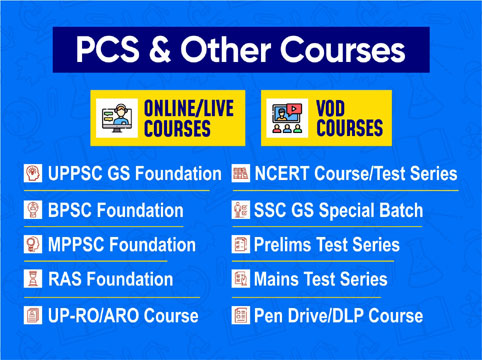
 Contact Us
Contact Us  New Batch : 9555124124/ 7428085757
New Batch : 9555124124/ 7428085757  Tech Support : 9555124124/ 7428085757
Tech Support : 9555124124/ 7428085757